| Name of hospital: | Date of inspection: | ||
|---|---|---|---|
| Inspection area: | |||
| Inspector's signature: | Co-Inspector's signature: | ||
Purpose: This document is recommended for use by infection control staff, medical personnel, ventilation technician, air-conditioning system maintenance worker, and environmental safety staff on a regular follow-up.
I.SARS Isolation Ward Management
1. Does the border space between general area and the isolation area of patients and medical supply completely isolated?
(1) Route of isolation area for patients and medical supply should be completely separated from the general area if a private isolation floor is available. If this mode is adopted in an open area, temporary partition walls that go from floor to ceiling could be used as a complete g separation of isolation and general area.
(2) It is desirable to have two separate dressing rooms for medical staff if facilities and space are available: one in uncontaminated area for entering isolation area and exiting rest area, and the other - one in contaminated area for exiting the isolation area and re-entering the rest area. Similarly, in order to minimize the potential risk of cross contamination, it is desirable to have two separate elevators: one for the transport of uncontaminated medical staffand supplies, and the other one for the transport of contaminated waste and patients.
(3) Should it be too difficult to distinguish between contaminated and clean area (uncontaminated), the other alternative is to alert medical staff by marking on the floor or walls to divide the area into three levels as Uncontaminated, Semi-contaminated and Contaminated. While staffs, goods and materials move from lower contamination level to a higher one, disinfection facilities are suggested to be installed and used before going through the boundary.
2. Do the movement of the personnel, and transport of material and waste in the separated areas being strictly controlled?
(1) A management system should be established and enforced to prevent cross entrance to contaminated/uncontaminated area. Warning signs should be posted properly at the boundary to prohibit cross entrance. Cross entrance is permitted only under specific conditions approved by the security guards.
(A) Appropriate communication channel and skills: It is suggested that intercoms and TV monitors be used to facilitate the communication. It is highly recommended to provide both spiritual and mental supports to the patients and their family, and hence enhance the patients' strength and desire for survival. Always ask about their feeling and things they need, record the details of the conversation in specific work forms, and then make sure to take all items needed to the isolation rooms as you enter it next time. Do not allow medical staff to respond to the unreasonable requests (for example: being asked to pass in and out of the isolation rooms frequently) of the patients and their family, and enter/exit the isolation rooms randomly in uncontrolled manner.
(B) As the medical staff entered the isolated wards, the following itemsshould be observed:
a. Ensure that all items of equipment and materials for medical treatment are ready. Stay calm and be alert.
b. Through intercoms, double check with the family to make sure that the quantity and items of equipment and materials that are to be brought into the wards are correct. Tell the family what you intend to do and what you expect them to do to assist you. (Ensure that all conversation was done prior to prior to entering the ward);
c. Check if the protection equipment works, including headgears, clothing for separation, eyeshades, three-layered gloves, shoes covers, the indicator of the negative-pressure gauge on the isolation door;
d. Unlock the isolation doors or turn on the electric switch; enter the preparative chamber as soon as possible (the door between the preparative chamber and the medical caring center will be closed immediately), stay in the chamber for longer than one minute to allow airflow become stable, deploy the disinfectant, and check all items of materials and equipment that you take with you once again;
e. If the smoke tube is available, use it the to ensure that the airflow of the crack of the door and its frame flows from the preparative chamber toward the inside of the isolated ward;
f. Return the smoke tube and enter the isolated wards rapidly (the door between the wards and the preparative chamber will be closed immediately).
(C) As the medical staff entered the isolated wards, the following should be observed: 1. Make sure that the relative position of the patients and themselves is advantageous to minimize the potential risk of exposure to harmful substance of the breathing zone (refer to the fifth item); 2. Be relaxed, breathe regularly, and avoid speaking. Talk softly if necessary to avoid the movement of muscles of the face and work tenderly to avoid sweating; 3.Ensure that things need to be done are done; 4. Perform the dangerous-actions that would produce spatters, such as drawing out the phlegm, at the very last moment before you leave the patient's room.
(D) As the medical staff leave the isolation rooms, the following should be obeyed: 1. Take off the outermost gloves slowly and calmly in the isolation rooms; 2. Leave the rooms and then move on r to the preparative chamber (the door between the isolation rooms and the preparative chamber will be closed immediately); 3. Disinfect all items in accordance with the three-grade protection procedure in the preparative chamber and take off the other gloves step by step; 4.Wait for longer than one minute to allowthe airflow becomes stable and let the contaminants and possibly the obnoxious odorthat were carried from the isolationrooms to be eliminated by the negative pressure system. Think of any deficiencies in the contamination protection procedures. 5. Step on the switch of the preparative chamber which leads to the medical caring center and enter the center rapidly (the door between the preparative chamber and the medical caring center will be closed immediately); 6.Lock the isolation room door or turn off its power supply.
The four key points mentioned above can be condensed and printed clearly on six posters for various stages of protection. They should be posted on the walls, with the bottom of the poster at 1.6 meter from the ground, at the following six different locations: 1.By the intercoms of the monitors in the medical caring center, 2.The space between the medical caring center and the preparative chamber 3.The space between the preparative chamber and the isolation rooms 4.By the sickbed, 5.The space between the isolation room to the preparative chamber, 6.The space between the preparative chamber to the medical caring center. These posters are intended to remind the medical staffof the safety and hygiene concerns even if they are exhausted the five and undernervous circumstances.
(2) According WHO, the virus of SARS can survive in the patients' excrement and urine. It is therefore suggested, that the sanitary workers must exercise extreme cautions while handling patients' human wastes and the containers, including the carts. They should be disinfected first as they are moved out from the isolation area after the wastes are sealed in order to minimize the potential risk of contamination.
(3) It is suggested that the disinfection should be conducted first as the wastes are moved out of the isolation areas, and, after the wastes were transferred to the transport carts, do it again by people handling the transport carts (as some of the harmful substance could possibly spills). The third disinfection should be executed when the carts are far away from the infected area. (This process should include the disinfection of the carts that transport the wastes from the isolation area, the ground along the transport path, and the walls which could possibly be contacted by the wastes during transportation).
3. Could switches on the wall, medical instruments and carts used by medical personnel become blind spots for prevention of contamination?
In order to avoid infection through hands, it is desirable to open the door with a foot-stepping mechanism at all possible contaminated entrances, such as entrance of quarantine units, pathway from preparation room to nurse station, and entrance of transferring patients to quarantine units. For medical instruments and carts that have been contaminated by patient's feces, urine, or body fluid, they should be treated as medical wastes, and, as such, should be disinfected and sterilized before leaving quarantine units or entering uncontaminated area to avoid accidental infection on staffs working at the nurse station.
4. Does the handling of waste affect the effectiveness of ventilation system?
Are the collection bags of waste completely sealed? Are waste-containerscovered with lids and are operated with foot-stepping trigger method? Is the waste exposed inattentively in the area where wind blows on, thus virus get diffused inside the rooms?
5. Do medical personnel stand in a correct position relative to the patients?
(1)General Rule:
When medical personnel standing against the air current it forms a recirculation zone in front of the medical personnel. If the contaminant exists in the recirculation zone, the concentration of harmful substance breathed into their mouths and noses could possibly be accumulated and increased. (See left illustration below)
2) When treating patients, medical personnel should avoid standing against air current and have patient stay in front of the medical personnel. If this is unavoidable, then change the patient's bed orientation and move the patient's head toward the ventilation outlet.
(3) It is suggested that medical personnel standing in a vertical direction to indoor air current, also adjust patient's bed as well to allow patient stay in front of medical personnel. (See right illustration above)
6. Is it possible to divide a single quarantine room into a number of units when it has to keep more than one possible cases in the same room under an inevitable circumstance?
In case of insufficient medical treatment resources and more than one patients of suspicious cases are forced to stay in the same room, sort out the most possible case and move that patient to the place near ventilation outlet and put other patients' beds in orders next to the door (inlet). Avoid keeping the most suspected patient next to the inlet.
II. Maintenance of HEPA Filters
1. Is the exhaust air from isolation ward treated by HEPA Filter?
(1)The exhaust air from isolation ward must be treated by HEPA first (Thefiltration efficiencyis 99.97% for the particles with a diameter of 0.3um.) before it was discharged outside. There should be no exception to this requirement.
(2)The HEPA Filter can be used in conjunction with an in effective auxiliary sterilizer, such asultraviolet (UVGI),ozone generator, etc., when available.
2. Is the exhaust system running continuously when a HEPA system is used by more than one isolation ward at the same time?
(1)When a HEPA system is used by more than one isolation ward simultaneously, the exhaust the system must be running continuously to avoid potential circulation of viruses through other wards.
(2)To ensure the normal power supply in case of an emergency power failure, the air conditioner of isolation zone should be parallel connected to an uninterruptible power supply (UPS).
3. Is the HEPA Filter replaced periodically?
(1)Follow the HEPA Filter replacement schedules established by the original manufacturer.
(2)If the original manufacturer cannot decide the filter replacement schedule, follow the experience accordingly, i.e., replace the filter every three months for exhaust HEPA and four months forair inlet HEPA..
4. Is the HEPA Filter used for an isolation ward alone replaced in a timely manner?
(1)If every isolation ward has its own HEPA Filter and theremaining lifespanis shorter than two weeks, replace it with a new one before a patient moves into the ward.
(2)Replace a new HEPA Filter seven days after the patient moves out the ward.Replacement of HEPA Filters poses potential risks of maintenance workers' exposed to SARS virus, and thus, should not be done too frequently.
5. Is the replacement of the HEPA Filter conducted safely?
(1)Follow the procedures as illustrated in the sketch for filter replacement: (1)Closes valves 1 and 2 and installs the new Filter A; (2)Opens valves 1 and 2 and conducts leakage test to ensure that the system is gastight; (3)Closes valves 3 and 4 and keep the Filter B in place for more than seven days, i.e., the duration that all SARS viruses are expected to be killed; (4)Removes the old Filter B by an employee with full protection against SARS (isolation suit, eye protection, respiratory protection, gloves, footwear), seals Filter B, and then treats it asmedical waste in accordance with applicable regulations.
(2)According to WHO, the virus survives longer in lower temperature (For instance,in temperature lower than 4¢FJ, the virus can survive up to 21 days without decreasing significantly). Thus, the replacement of HEPA Filters poses a potential risk of exposure to maintenance workers. It is therefore suggested that the filter replacement area be treated as contaminated zone. The removed old HEPA Filter should be handled/disposed of properly, and the maintenance workers should be reminded to disinfect themselves thoroughly.
6. Is the function of HEPA Filter monitored properly?
(1)HEPA Filter is ahigh pressure resistant element and the pressure dropincreases with time, especially if the environment is dusty. We therefore suggest that adifferential pressure gauge be installed tomonitor the variation of the pressure drop across the filter. Alternatively, an automatic control system can be installed for closed-loop monitoring and maintains a constant pressure drop across the filter.
(2)Under normal operation, the pressure drop of HEPA Filter must be between the initial and final pressure drops. The initial pressure drop is the one when a new HEPA Filter is installed, and the final pressure drop is the one when the filter reaches its recommended life. If the pressure drop of a newly installed system is lower than that of the filter, it indicates that the leak occurred at the time of installation). On the other hand, if the pressure drop increases substantially, it signals the pending failure of the ventilation system due to excessive resistance. The system is functioning abnormally if the operation pressure drop falls outside the range of initial and final pressure drops.
(3) To ensure that a HEPA system works properly, it can be designed based on the experience and professional judge of HVAC engineers or specialist, if the information on the initial and final pressure drops is not available from the manufacturer, and no standards are specified by building codes or other regulations. (It is a desirable to mark three color-coded zones on the pressure gauge to indicate low, normal, and high pressure drops. For example, yellow, green, and red zones can be marked on a Magnehelic pressure gauge)
III.HVAC (Heating, Ventilation, and Air Conditioning) Design and the Operation
1. Is the air that enters the inlet of air conditioner 100% fresh air and contains no re-circulated air?
(1)Common Practice: For energy saving, some older air conditioner systems usually take a certain fraction of the cold air from an isolated zone, mixed with fresh air, and then return it to the same zone again. This practice poses a potential risk of spreading the virus to other spaces in the hospital.
(2)We suggest that air conditioner system uses fresh intake air only: The air from the isolated zone must be treated by HEPA and all to be discharged outside. The air which enters the inlet of system must be 100% fresh air.
2. Is the gas flow of preparation room designed correctly?
(1)Common Practice: The preparation room, which is located between isolation ward and nurse station, provides a space for nursing staff to gear up protective equipments prior to entering the isolation ward.
(2)The air of the preparation room should flow from nurse stationtoisolation ward. If the direction of air flow is reversed the contaminated air from the isolation ward may blow outward to other spaces, posing a potential risk of cross contamination.Wesuggest that a smoke test tube be used to verify the properairflow direction.
3.Are air flow patterns inside the ward properly designed?
(1) Common Practice: The primary air flow inside the ward should be parallel, stable, low speed, uniform, and non-turbulent to avoid the hazard material accumulation. From the air diffuser inside the ward, the primary air flow passes through the area adjacent to the patient, mixed with hazard materials, then drift toward the venting outlet. The secondary air flow runs through the crack underneath the door and its frame to maintain a negative pressure inside the ward so as to prevent the dispersion of hazardous materials to outside of the ward.
(2) For air inlet, it is suggested to install 2 - 3 fresh air diffusers on the wall side by side above the door. If this configuration is infeasible due to limited wall space, the air inlet, alternatively, can be installed in the ceiling adjacent to the door. For a given designed air circulation for the room, multiple air diffusers are more desirable than a single one for better uniform air distribution.
(3) The air outlet (i.e., the polluted air flows toward HEPA) should be installed at the wall or ceiling opposite to the inlet, with the air flow slightly more than the inlet flow. (Comment by Chuck Chang: The outlet air = Inlet air through the diffuser + Air flow through the crack below the inlet door. This is needed to maintain a negative pressure inside the ward).
(4) The patient's bed should be located as near as possible to the air, with the headboard or pillow placed perpendicular on the outlet side. Based on this orientation of air handling system and the patient's bed position, the medical workers are required to stand on both sides of bed and avoid standing at the head and tail of bed. This will help to reduce the potential risk of medical staff's exposure to the virus since lower aerosol concentration near their nose and mouse is expected.
4. Does the contaminated air use the same recycle air duct ofthe air conditioning system for general area?
(1) Common Practice:The pressure balance of the ventilation system for the quarantine zone should be solely used for the zone. It should not be mixed with the air conditioning for the general area.
(2) If a quarantine zone is temporarily established in an area where re-circulated air outlets for general area air conditioning system already exist, the outlets should be sealed or re-connected to the re-circulated air ducts of the ventilation system dedicated to the quarantine zone. This will prevent the potential risk of mixing the contaminated air from the quarantine zone with the air handled by the air conditioning system for the general area.
5. Are designed air flow rates of quarantine ward adequate?
The designed exhaust air flow rate of quarantine ward should greater than the designed intake air flow rate, assuming both the inlet and outlet air ducts are of the same size. As a general practice, a flow rate of 1.2 times intake air flow rate is suggested for the outlet.With this design, the air should flow from outside into the ward when the door of quarantine ward is completely opened.
6. Is negative pressure of quarantine ward sufficient?
(1) Conversion factor: 1 in Aq = 25.4 mm Aq =249 pa
(2) Place the pressure checkpoint close to the door seam of the lower half quarantine ward door is suggested, in order to reflect airflow direction as accurately as possible.
(3) A static pressure difference of 0.1" water column between inside and outside of the ward is suggested (This is the engineering design specification of Exxon Mobil company in the States for industrial situation to prevent toxic substances from escaping to outside. Taiwan may want to consider these criteria). Do not open the door of quarantine ward too frequently.
(4) The pressure differential readings mentioned above should be clearly indicated on a pressure gauge installed on the outside wall of the quarantine ward for people to visually read and confirm the reading. A pressure gauge with color-coded performance zones is desirable for continuous monitoring to the system. (Example, Yellow = Inadequate, Green = Normal Operation, Red: Excessive).
7.Is air change rate of quarantine ward sufficient?
A quarantine ward should be designed with an air change rate of 8-12 times/hr, or in accordance with the suggestion made by the Center of Disease Control, Department of Health, Executive Yuan, Taiwan.
8. Static air pressure planning of quarantine zone.
A relatively positive pressure should be provided from nurse station to the quarantine ward corridor (or preparation room), and from the quarantine ward corridor (or preparation room) to the inside the quarantine ward. Use a flow indicator to check air flow..
9. Should windows of quarantine ward be sealed completely?
If windows of quarantine ward are opened, contaminated air will leak out and will seriously affect the negative pressure setting. Therefore, all windows of the quarantine ward should be completely sealed.The door seam of quarantine ward door should be unsealed for checking the negative pressure and air flow.
10. Is design of the Virable Air Volume (VAV) system reasonable?
Following are the VAV system design principles:
(1) Either the intake air or outlet air can be controlled by VAV, but not both simultaneously. For example, if the inlet air is controlled by VAV, then the outlet air should use a fixed air volume, and vice versa.The design of fix air volume side should satisfy the air change requirement. If both intake air and outlet air use VAV system, it will make the system difficult to control, unstable, and affect the quarantine effect.
(2) In designing an effective ventilation system for the quarantine ward, the first priority is to make sure that a sufficient air volume is provided, either by automatic or manual control system, to maintain negative pressure inside the ward. The temperature and humidity are secondary considerations.
IV. Ventilation Duct Design and Operation
1. Does an adequate distance kept between the outlet of contaminated air and the inlet of fresh air?
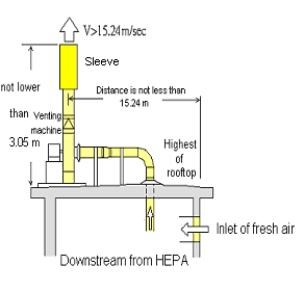
A horizontal distance of at least 15.3 meter or more should be maintained between the outlet of contaminated air and the inlet of fresh air based on typical building configurations of hospitals in Taiwan.
2. Isthe venting outlet located at the highest position of building?
All venting outlets should be located at rooftop and far away the elevator or the open space of other protruding rooftop. In addition, the venting outlet should be located as far way as possible from the inlet of fresh air as mentioned earlier.

3. Does the venting outlet have obstructions inside?
A sleeve can be used in the design of venting outlet so that the rain could be discharged via the interval between inner and outer sleeves. A shelter or canopy also can be used as long as the air outlet is not obstructed.
4. Does the distance from the rooftop to the venting outlet provide sufficient space for effective air dispersion?
The height from the rooftop to the venting outlet should be at least 3 meter or more. The venting direction should be vertical and upward.
5. Does the speed of air stream from venting outlet is adequate for proper air dispersion?
The speed of air stream from venting outlet should be at least 15 m/sec or more and pointed vertically upward in order to increase the efficient height of venting and increase the dispersion and mixing effects. (This is equivalent to increase the effective height of a smoke stack).
This document is jointly developed and reviewed by a number of experts and organizations. Kenneth M. Wallingford of the US National Institute of Occupational Safety and Health (NIOSH) and Gregory A. Burr of the US Centers for Disease Control and Prevention (CDC) Taiwan in May 2003 to assist the SARS epidemic control. Through the coordination of Dr. Chun-Hsien Lee,Center for Disease Control Taiwan, R.O.C.with Institute of Occupational Medicine and Industrial Hygiene, College of Public Health, National Taiwan Universityand The Institute of Occupational Safety and Health, Council of Labor Affairs, Executive Yuan, Taiwan, R.O.C. this development of this document was evolved.
Following the field visits and investigations of a number of SARS treatment hospitals (including byNational Taiwan University Hospital,main branch hospital and Tamshui branch hospital ofMackay Memorial Hospital, Taipei county San-Chung Hospital , Miao-Li General Hospital of department of health, and Chu-Tung hospital) by the experts, Researcher Shuen-Chih Wang initiated the development of the document and seeks advices from the following individuals, including t Kenneth M. Wallingford, Dr. Chun-Hsien Li, doctor candidateTa-Yuan Chang, from Kenneth M. Wallingford, Gregory A. Burr, Chang-Chuan Chan, Jia-Ming Lin, Fung-Chang Sung, Chun-Wan Chen, Huey-Jen Su, Perng-Jy Tsai ,Chih-Shan Li, Yao-Hui Huang, Sun-I Wang, Jung-Der Wang, Shou-Chen Chang, Yi-Chang Lin, Cheng-Ping Chang, Ching-Nien Chang (the chief nurse in isolated sickroom on first floor of Mackay memorial hospital), Yu-Kang Chen, Kee-Chiang Chung, Chih-Chieh Chen, Yi-Shiaw Huang, Tung-Sheng Shih, Sen Chen, Kuo-Hsiang Yang, and Wen-Yu Yeh. The document was subsequently reviewed by the Department of Occupational Medicine and Department of Industrial Hygiene of National Taiwan University, Center for Disease Control, and Institute of Occupational Safety & Health respectively and on 8 th , May, 2003, all parties agreed to adopt the guidelines. For more details or any questions, please contact Shuen-Chih Wang, the main author, by telephone at 886-02-2660-2600 # 209, or by email, wangsj@mail.ilosh.gov.tw .
(This document was critically reviewed by Dr. Hsing-Chi Chang, an Industrial Hygienist with the Medicine and Occupational Health Department in a leading world-wide petrochemical company in the US)
- Source:ILOSH
- Last updated:111-08-18
- Count Views:



